Understanding and Managing Autoimmune Diseases
Autoimmune diseases can be regarded as a group of disorders where the body’s immune system mistakenly attacks its own tissues. These situation affect millions of people worldwide and can impact various parts of the body, leading to a wide range of symptoms. While the exact cause of autoimmune diseases remains difficult to track down, understanding these conditions and implementing effective management strategies can remarkably enhance quality of life and overall health. This article explores the nature of autoimmune diseases, their common types, causes, symptoms, and comprehensive management strategies.
What Are Autoimmune Diseases?
Autoimmune diseases occur when the immune system, maped out to protect the body from harmful invaders like bacteria and viruses, mistakenly targets healthy cells. This unwarranted immune response can affect different organs and tissues, leading to inflammation, tissue damage, and a host of symptoms. There are over 80 recognized autoimmune diseases, each with unique characteristics and challenges.
Common Types of Autoimmune Diseases
- Rheumatoid Arthritis (RA)
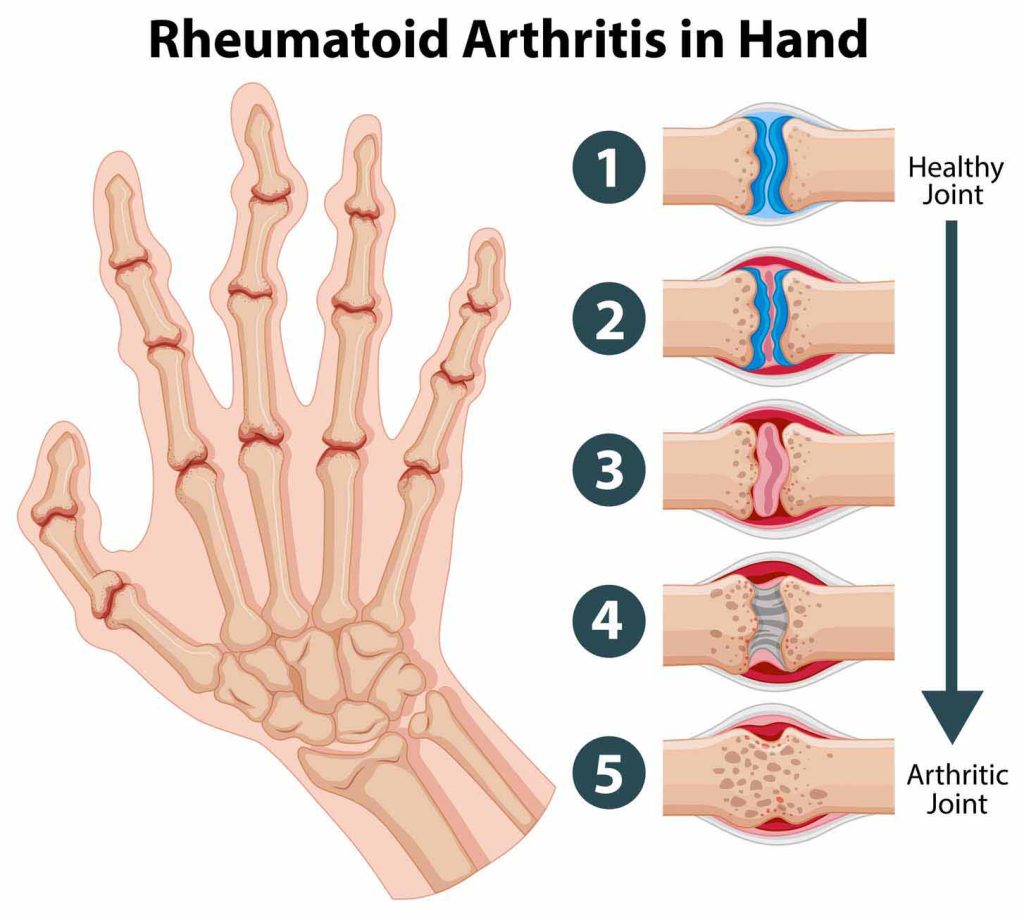
- Description: A chronic inflammatory disorder primarily affecting the joints.
- Symptoms: Joint pain, swelling, stiffness, and potential joint deformity over time.
- Impact: RA can lead to severe joint damage and disability if not properly managed.
2. Systemic Lupus Erythematosus (SLE)
- Description: A systemic disease affecting multiple organs, including the skin, joints, kidneys, heart, and brain.
- Symptoms: Fatigue, joint pain, skin rashes (notably a butterfly-shaped rash on the face), and kidney problems.
- Impact: SLE can cause widespread organ damage and significantly affect quality of life.
3. Type 1 Diabetes

- Description: An autoimmune condition where the immune system attacks insulin-producing beta cells in the pancreas.
- Symptoms: High blood sugar levels, frequent urination, excessive thirst, and weight loss.
- Impact: Without insulin, the body cannot regulate blood sugar levels, necessitating lifelong insulin therapy.
4. Multiple Sclerosis (MS)
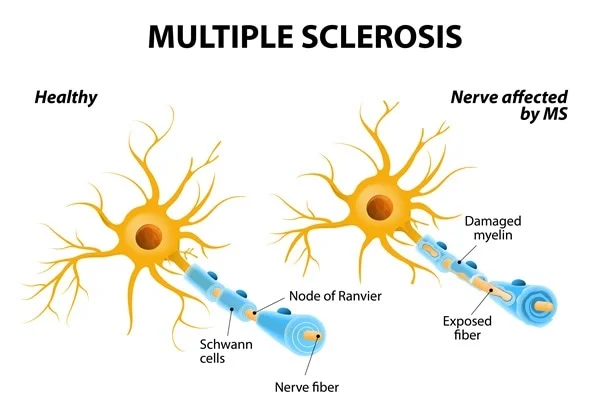
- Description: A disease in which the immune system attacks the protective covering (myelin) of nerve fibers in the central nervous system.
- Symptoms: Muscle weakness, coordination and balance issues, numbness, and vision problems.
- Impact: MS can lead to progressive physical and cognitive disability.
5. Hashimoto’s Thyroiditis

- Description: An autoimmune disorder causing hypothyroidism (underactive thyroid).
- Symptoms: Fatigue, weight gain, cold intolerance, and depression.
- Impact: Untreated hypothyroidism can lead to serious health problems, including heart disease and mental health issues.
6. Graves’ Disease

- Description: An autoimmune condition causing hyperthyroidism (overactive thyroid).
- Symptoms: Weight loss, rapid heartbeat, anxiety, and bulging eyes.
- Impact: If untreated, it can lead to severe complications such as heart problems and brittle bones.
7. Celiac Disease

- Description: An autoimmune disorder triggered by the ingestion of gluten, leading to damage in the small intestine.
- Symptoms: Digestive issues, anemia, fatigue, and nutrient deficiencies.
- Impact: Long-term complications include malnutrition, osteoporosis, and an increased risk of intestinal cancers.
Causes and Risk Factors
The exact cause of autoimmune diseases is not fully understood, but several factors are known to contribute to their development:
- Genetics: A family history of autoimmune diseases can increase susceptibility. Specific genes have been linked to higher risks of certain autoimmune conditions.
- Environmental Triggers: vulnerability to infections, certain medications, chemicals, and toxins can trigger autoimmune responses in genetically make vulnerable individuals.
- Hormonal Factors: Autoimmune diseases are more frequent in women, suggesting that hormonal differences play a role. Hormonal changes during pregnancy or menopause can impact immune function.
- Diet and Lifestyle: Poor diet, lack of exercise, chronic stress, and smoking are linked to an increased risk of autoimmune diseases.
- Infections: Certain viral or bacterial infections can act as triggers for autoimmune responses.
Symptoms of Autoimmune Diseases
Symptoms of autoimmune diseases vary widely depending on the specific condition and the organs or tissues affected. Common symptoms include:
- Fatigue
- Joint pain and swelling
- Skin rashes
- Digestive issues
- Unexplained weight changes
- Muscle weakness
- Hair loss
- Numbness and tingling in the hands and feet
- Difficulty concentrating
These symptoms can overlap with other health conditions, making diagnosis challenging. Accurate diagnosis often requires a combination of medical history, physical examinations, blood tests, and imaging studies.
Managing Autoimmune Diseases
While there is no cure for autoimmune diseases, effective management strategies can help control symptoms, reduce inflammation, and improve quality of life. Key management approaches include:
- Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Help reduce inflammation and relieve pain (e.g., ibuprofen, naproxen).
- Corticosteroids: Powerful anti-inflammatory drugs used to control severe inflammation (e.g., prednisone). Long-term use may have side effects.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Slow disease progression, particularly in rheumatoid arthritis (e.g., methotrexate, hydroxychloroquine).
- Biologic Agents: Target specific parts of the immune system to reduce inflammation (e.g., adalimumab, etanercept).
- Immunosuppressants: Suppress the immune system to prevent it from attacking healthy tissues (e.g., azathioprine, cyclosporine).
- Lifestyle Changes
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports immune function and reduces inflammation. Avoiding processed foods, sugar, and unhealthy fats is also beneficial.
- Regular Exercise: Physical activity helps reduce inflammation, improve joint mobility, and boost mood. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Stress Management: Chronic stress can exacerbate autoimmune symptoms. Techniques such as mindfulness, meditation, yoga, and deep breathing exercises can help manage stress levels.
- Adequate Sleep: Quality sleep is essential for maintaining optimal health and hormonal balance. Aim for 7-8 hours of uninterrupted sleep per night.
- Dietary Supplements
- Omega-3 Fatty Acids: Found in fish oil, flaxseeds, and walnuts, omega-3s have anti-inflammatory properties.
- Vitamin D: Deficiency in vitamin D has been linked to autoimmune diseases. Supplements can help maintain adequate levels.
- Probiotics: Support gut health and immune function. Found in yogurt, kefir, and fermented foods.
- Alternative Therapies
- Acupuncture: Can help manage pain and improve overall well-being.
- Massage Therapy: Reduces stress and muscle tension.
- Herbal Medicine: Some herbs, like turmeric and ginger, have anti-inflammatory properties. Consult with a healthcare provider before starting any herbal supplements.
- Regular Medical Check-ups
- Monitoring: Regular check-ups with a healthcare provider can help track disease progression and adjust treatment plans as needed.
- Early Intervention: Prompt treatment of symptoms can prevent complications and improve outcomes.
Autoimmune diseases present a complex challenge due to their varied symptoms and unpredictable nature. However, understanding these conditions and adopting a comprehensive management approach can remarkably improve quality of life for those affected. By combining medical treatments with lifestyle changes, dietary adjustments, and stress management techniques, individuals can effectively manage their autoimmune conditions and lead fulfilling lives. Regular communication with healthcare providers is important to tailor treatment plans to individual needs and ensure optimal care.